Introduction
Medical malpractice is a major cause of mortality and morbidity globally, with significant consequences for healthcare systems, communities, and providers. Malpractice claims negatively affect physicians’ well-being, leading to burnout, depression, and suicidal thoughts, as demonstrated in a study including 25,000 surgeons.1
Despite physicians valuing legal knowledge, their understanding of medical law remains limited. Therefore, integrating medical law training in undergraduate and postgraduate education is crucial.2 Numerous researchers have advocated for incorporating medical law and ethics fundamentals into medical school curriculums. Attaining this knowledge enhances medical professionals’ critical thinking skills and decision-making prowess throughout their practice, thereby enabling them to address diverse clinical challenges in an ethically, legally, and professionally justifiable manner.3
Incorporating Islamic Medical Jurisprudence into the medical school curriculum enhances the caliber of medical practice.4 It standardizes general practice within Islamic communities that regard the Quran and Sunnah of Prophet Muhammed as fundamental sources. In 2005, the Saudi Arabian government implemented the Medical Liability Law, establishing a legal framework for patients seeking remuneration due to medical malpractice or negligence.5 Nevertheless, a notable increase in legal, medical claims was observed by the Sharia Medical Panels (SMP), with reported cases escalating from 2002 in 2012–2013 to 3043 in 2015–2016.6 Consequently, there is a critical necessity to reinforce and safeguard the community’s rights concerning medical errors in healthcare environments.
To augment healthcare quality and bolster patient safety, the Saudi Arabian government instituted the Saudi Commission of Health Specialties (SCFHS) in 1992.7 The SCFHS is responsible for regulating healthcare professions within the nation, licensing practitioners, and addressing diverse facets to ensure high-quality healthcare training. The Saudi Board of Emergency Medicine (SBEM) program, initiated in October 2001, is among the most prominent residency-training programs governed by SCFHS.8 The SBEM curriculum adheres to the Can MEDS9 roles framework competencies encompassing medical expert, communicator, collaborator, manager, health advocate, scholar, and professional. The objectives of this study include an investigation into the existing educational approaches of legal and bioethical topics within the Saudi Board of Emergency Medicine (SBEM), as well as an examination of key stakeholders — program directors and trainees — perceptions regarding the incorporation of a legal and bioethical education module into the current curriculum.
Aim
The objective of this study is to investigate the present educational methodologies concerning legal and bioethical topics within the Saudi Board of Emergency Medicine (SBEM) curriculum and to examine the perspectives of significant stakeholders (including program directors and trainees) on the incorporation of a legal and bioethical educational module into the existing curriculum.
Objectives
- Examine the current pedagogical approaches in SBEM concerning legal and bioethical issues, encompassing: selected subject matter, instructional methods, assessment methods, resource materials for study guides, and roles of participating individuals.
- Investigate the perspectives of both program directors and trainees within SBEM regarding incorporating a well-established legal and bioethical module into the existing curriculum.
- Identify the most appropriate instance for incorporating the legal and bioethical module into the current SBEM curriculum.
Methods
Study Design and Sampling
The study was conducted utilizing a qualitative research methodology. Key stakeholders, whose perspectives were pertinent to the objectives of this study, were identified and engaged in the process. These stakeholders included:
- SBEM program director: As delineated by the SCFHS,10 a proficient, licensed specialist responsible for overseeing a specific training program within a training center.
- Trainee: As stipulated by the SCFHS,10 an individual who has been accepted into and enrolled in an approved training program governed by the SCFHS.
A purposive sampling technique was used. A total of 19 participants (comprising seven program directors and 12 trainees) were involved in this study, originating from various training centers throughout the Kingdom of Saudi Arabia. The trainees represented a range of training levels, spanning from level one through to level four.
Data Collection
The approach utilized for data gathering contained comprehensive, in-depth interviews. Participant recruitment endeavored through various channels such as email and WhatsApp invitations, direct personal communication, and telephonic conversations. The lead researcher is an emergency medicine consultant with over five years of experience in the field and serves as the deputy program director at her training center. Utilizing her professional connections, she reached out to program directors. Subsequently, she contacted program educational coordinators and directors for access to the trainees. In some cases, she directly approached trainees within her workplace.
The lead researcher primarily executed the interviews utilizing virtual means, supplemented by nine in-person interviews conducted at the participant’s place of work. Upon consenting to participate in the study, the participants underwent interviews lasting between 30 to 60 minutes, with each session being audio-recorded and transcribed verbatim.
The interview questions were devised in accordance with the research objectives by the lead researcher. Two Medical Education specialists assessed these inquiries (refer to Appendices 1 and 2 for further details). Separate interview guides were created for program directors and trainees, given their distinct perspectives. The questions were designed to be open-ended, thereby encouraging the provision of extensive information. Throughout the interviews, supplementary questions were posed as needed to elicit clarification and additional specifics.
The participants were not consulted regarding the findings, except in a single encounter. This was done to address one trainee’s feedback about the presence of a designated module covering ethical and legal issues. The approach taken was professional in nature.
Additional demographic variables were gathered, incorporating factors like gender, age, geographical area, educational institution, number of trainees at each location, program directors’ duration of experience and sub specialization, and trainees’ level of education. The investigation’s questions examined the existing bioethical and juridical instruction within the scope of SBEM from both program directors’ and trainees’ standpoints. Moreover, it aimed to discern their opinions concerning integrating a bioethical and legal pedagogical module into SBEM’s future curriculum and identify the optimal timing for such a module’s introduction.
Data Analysis
Data analysis was conducted concurrently with data collection. The lead researcher meticulously transcribed each recorded interview. Utilizing a constant comparative method, data were continually assessed and analyzed, culminating in theoretical saturation. Initially, two research team members independently examined the first eight transcripts, identifying emerging themes and conducting open coding. Subsequently, they convened to discuss and compare their results, ultimately devising the initial open coding structure consisting of numerous codes and sub-codes. As additional interviews took place, this coding framework was implemented by the research team members and modified as new topics emerged. This approach was applied to the remaining interview transcripts.
The researcher continued the interviews until they detected a consistent pattern in the responses from the participants. When they observed this recurrent pattern, they declared that data saturation had been achieved and decided not to proceed with any more interviews.
Subsequently, a third research team member reviewed the open codes, progressing to axial and selective coding alongside the rest of the team. The main themes and subthemes were then established, concentrating on the needs assessment for incorporating a bioethical and legal module into the existing SBEM curriculum from the perspective of two primary stakeholders (program directors and trainees). Finally, connections among categories were identified, and categories were refined to determine central themes. The research team engaged in discussions to evaluate thematic categories and their interrelationships.
Ethical Approval
The study received approval from the Institutional Ethics Committee of King Abdullah International Medical Research Center (IRBC/1933/20). Before conducting interviews, verbal consent was obtained from each participant, encompassing their involvement in the study and video and audio recordings. Participation was voluntary; thus, individuals faced no penalties for refusing to take part or declining to answer specific questions. No identifiable information, such as names, email addresses, or IP addresses, was collected. Transcript data, video footage, and audio recordings were stored securely without identifiers on the researcher’s computer. Following data analysis, the researcher deleted the recorded videos and audio. No transcripts were sent back for review; there were no repeated interviews or refusal to participate in the research.
Results
The study encompassed 19 participants, seven program directors, and 12 trainees (n=19), with a gender distribution of 13 males and six females. Most program directors are associated with educational institutions that accommodate over 20 trainees. The average experience of the program directors as emergency medicine consultants range between 11 and 15 years (Figures 1 and 2). Geographically, one program director was interviewed from Jeddah and the Eastern Province, while the remainder were based in Riyadh. Of the trainees, one hailed from the Eastern Province, one from Jeddah, and the rest from Riyadh. Subspecialties among program directors included Disaster Medicine, Point of Care Ultrasound, and Toxicology. Additionally, two program directors possessed Master’s degrees in Medical Education and fellowships in Medical Simulation. Trainee participants spanned various training levels; five junior and seven senior-level trainees were interviewed, aged between 25 and 30.
Figure 1 Number of trainees in the training centers. Most trainees participating are from training centers with over 20 trainees. Among the centers, 14.3% accommodate 11 to 15 trainees, and 14.3% have fewer than six trainees. |
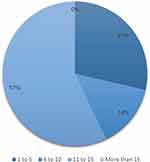 | Figure 2 Program Directors’ Years of Experience: The majority of program directors in the study have over ten years of experience as consultants in emergency medicine. Of the participants, 29% had less than 5 years of experience, while 14% had between 6 to 10 years of experience. |
Existence of Identified Educational Module for Bioethical and Legal Subjects in the SBEM and the Current Educational Practice
All The program directors (PD) and 11 trainees (T) stated that the Saudi Board of Emergency Medicine curriculum lacked identified, well-structured official modules to cover the bioethical and legal subjects. For example, one program director said:
I do not believe that there is a part of the official curriculum for the SABEM “the scientific council makes that of the program”; that curriculum does not include a legal module. (PD1)
And the other one said:
Officially in the Saudi board, there is no curriculum for law and bioethics. (PD2)
In this regard, all trainees had the same perception except for one trainee who wrongly assumed that the elective administration and leadership module included legal and bioethical subjects. Therefore, the program director who supervised this module clarified the module content, which focuses on leadership and management skills and lacked bioethics and medical law subjects. For example, one trainee said:
There is no designated or identified ethics module, but as trainees, we try to fill the gaps from the training consultants’ tips or textbooks to cover those subjects. Even during educational activity, the legal and bioethical subjects are not frequently visited. (T3)
When I face any ethical challenge, I approach the most senior person on the shift and look for their guide, as we do not have a fixed reference. (T7)
The data were analyzed using qualitative content analysis, and four themes and five sub-themes emerged (Table 1).
 | Table 1 The Themes and Subthemes That Emerged from Participant Feedback Regarding Integrating a Bioethical and Legal Educational Module in the Current SBEM Curriculum |
Theme One: Planning the Current Bioethical and Legal Educational Activities in the SBEM
The participants described the current bioethical and legal educational practice and their responses generated four subthemes:
The Control of Current Educational Activities
Despite the absence of an organized bioethical and legal module, most of the program directors take the lead in planning and executing educational activities to cover bioethical and legal subjects out of the belief of their value.
We are doing this because we believe it is important, and we are not doing it because we must do it, or it is part of the training…The explicit training instruction that we are seeking (PD1)
Most training centers devote particular time and speakers to introduce the trainees to everyday legal and ethical matters along with their privileges, rights, and duties at the beginning of their training to avoid legal liabilities. The SCFHS designed a special pamphlet to guide the trainees’ professional and general ethical practice. Moreover, the program directors include some ethical and general legal subjects during the weekly academic activities. However, they are purely out of personal effort and need to be better organized.
There is one pamphlet from the SCFHS which is available on the website to cover bioethics; there was one online lecture during the cluster 2 orientation, targeting the new trainees; however, it was not very beneficial and mainly described the bylaws (T4)
During the orientation period, we met one of the admin representatives who described to us what are our privileges and rights (T6)
Role of Program Directors, Trainers, and Senior Trainees in the Educational Process
The participants described the variable origins of the educational activities. Program directors decide most of the subjects based on their observations and experience. Some subjects were initiated based on the recommendation of other trainers, senior trainees, and scientific committees’ recommendations. A few topics were suggested by experienced speakers who had legal or administrative backgrounds.
All the program directors in the eastern province (more than one program director) meet with the chief of trainees to decide the subjects that should be covered (T5)
The participants described the varying roles of the program directors and trainers in the educational process of the bioethical and legal subjects. Some acted as bedside teachers who dealt with legal and bioethical dilemmas during their daily practice as teaching opportunities for the trainees. Others served as leaders who made sure to keep their trainees updated regarding the policies and procedures, ensure that their behaviors reflected a high level of professionalism, and correct their behaviors if needed. And some assumed the mentor role, who passed their personal experiences to the trainees. In some training centers, the senior trainees have educational roles where they arrange lectures for the junior ones focusing on general medico-legal subjects.
Teaching during clinical practice always happens even if there is no curriculum or clear requirements from the SCFHS; they always discuss those matters during the clinical practice, either from trainers’ personal experience. If something happens, they react directly and give immediate feedback. (PD5)
Lack of Awareness
Given the limited exposure to bioethical and legal aspects, the majority of participating trainees exhibited an unclear understanding of the educational process, particularly among junior members.
Theme Two: Teaching Methods and Guiding Resources in Bioethical & Legal Education
Instructional Method
Participants mentioned a few educational methods used in the SBEM to deliver legal and bioethical subjects. They include lectures, case-based discussions, online courses, bedside teaching, and simulation-based activities. The most frequently used method was case-based discussion, demonstrating real cases from different training centers.
Last year we did a communication case-based discussion session, and we had scenarios during the academic activity. We presented 5 cases in the form of play then we discussed how to deal with such cases and what are the consequences of them, we did it last year, and we are planning to do it this year (PD 6)
Guiding Educational Resources
The participants listed the current used guiding resources to cover the bioethical and legal subjects. They include a reference from SCFHS, eg, the online pamphlet, scientific publications, eg, journal articles and Emergency Medicine textbook) and online resources. In the participants’ opinions, those resources have their disadvantages. For instance, they lacked legal subjects and were incompatible with the Islamic community.
Despite the extensive details about bioethics and particularly the law in our textbooks, we cannot use them to sort out all the dilemmas we may face in our daily clinical practice. We need to have resources that cover our national Islamic law and are acceptable to our Muslim community (T3)
Theme Three: Current Assessment Methods in Bioethical & Legal Education
The responses from participating program directors indicated a need for a formative assessment approach to gauge trainees’ understanding of bioethical and legal concepts within SBEM. Despite the presence of some ethical and medicolegal components in the final written and oral board examinations, it is challenging to accurately determine trainees’ actual performance in these areas, as the exam results are presented as an aggregate rather than broken down into individual elements.
No formal assessment. I do not think those subjects are included in the SCFHS exam; however, during the case-based discussion, there is no standard assessment method to assure the residents’ comprehension of what has been discussed (PD7)
Theme Four: Opinions Regarding Integrating Bioethical & Legal Educational Module in SBEM
All participants (program directors and trainees) endorsed incorporating a bioethical and legal component into the existing SBEM curriculum. Some proposed the formation of an interdisciplinary team, comprising legal and medical professionals, to develop and instruct this mo. In contrast, others asserted that medical experts with legal expertise could successfully manage it.
I am pushing toward this, to have more medicolegal lectures in our educational activity. I even talked to our program director to include more ways to cover bioethical and legal subjects. I did not suggest a designated module. However, I was looking for more lectures and interactive sessions or seminars on this matter. I wish to have an ethics day which is like the research day, as we know very little about this subject (T3)
It is highly needed if your scale is ten, so it is ten or even 10+ because we have a huge deficiency in our curriculum since I was a trainee until now. (PD4)
We need someone who has the time, accreditation, and knowledge about that, and we need it to be feasible to be applied and simplified to trainees’ level. (PD4)
The participants expressed diverse viewpoints on the most suitable timing for incorporating the bioethical and legal components into the existing SBEM curriculum. Some propose its introduction early in the clinical experience, even during the internship phase. In contrast, others advocate for its integration later during training to prevent overburdening the junior trainees.
We should not overwhelm the juniors with the information they will not frequently use in their practice. (T2)
It should be started early in clinical life, even before graduation from medical school; the internship is the most suitable time for it, where the medical knowledge starts to be integrated with the clinical practice. Or it can be rooted in the junior years and will be continued till graduation, where it will be revisited again and again with more details. (T3)
Discussion
Our data elucidates the academic methodology concerning bioethical and legal subjects within the SBEM. It also unveils the necessity for a distinct, meticulously organized, and official module addressing bioethics and medical law principles within the SBEM curriculum. This is not an isolated issue, as numerous medical schools in Saudi Arabia lack structured medical jurisprudence curricula.4
Ethical and legal principles play a significant role in clinical practice, shaping various aspects for patients and healthcare providers. A better understanding of these principles minimizes liabilities and promotes interdisciplinary collaboration.11
On the other hand, a lack of such understanding and inadequate adherence to ethical standards and medical legislation could adversely impact the healthcare professional.12 Therefore, most of the program directors and other trainers perceived that need and acted beyond their typical instructional duties to fill the gap in the trainees’ knowledge.
Various disciplines are involved in the clinical training process, including training centers and the SCFHS. Participants outlined their endeavors to familiarize trainees with ethical and legal fundamentals despite differing objectives. Training centers operate under different regulations, as they adhere to different ministries. Nonetheless, they acquaint their trainees with associated legal frameworks and ethical guidelines through concise introductory lectures delivered by legal affairs experts. However, trainees argue that these efforts require improvement to address their needs effectively.
Conversely, SCFHS establishes general regulations addressing fundamental bioethical and legal queries encountered by healthcare providers during clinical practice. These guidelines are accessible in a written manual on the SCFHS website. Program directors consider the current manual outdated, primarily focused on bioethical issues, and inadequately advertised, as most participants were unaware of its existence.
Enhanced coordination between the SCFHS and training centers could facilitate the establishment of a unified national legal and ethical framework guided by the Ministry of Justice’s regulations under the Saudi Health Council’s supervision. This collaboration may standardize clinical practice across various health sectors and optimize resource allocation.
The findings from our study demonstrated that the ethical and legal topics encompassed within SBEM were derived from various sources rather than being based on established and consistent standards. The origins of these topics can be summarized as follows:
- The fundamental Islamic Bioethical and medicolegal standards that all trainees must acquire prior to completing their studies.
- Observations gathered by program directors and trainers during their clinical practice, focusing on frequently occurring issues they hope trainees will prevent in their future work.
- Singular incidents that program directors and trainers view as valuable learning experiences and impart to their trainees.
- Personal experiences shared by program directors and trainers themselves.
- Hospital documents related to mortality and morbidity cases, legal claims, and patient complaints.
Numerous global medical institutions have experimented with incorporating methods such as small group discussions, mock trials, and interdisciplinary models for teaching legal subjects.13 In contrast, SBEM educators, which include program directors, trainers, and senior trainees, have utilized several approaches to deliver bioethical and legal topics to trainees, encompassing case-based discussions, lectures, and simulations. Among these strategies, case-based discussions have achieved the highest level of familiarity. Although the participants were unable to justify this preference, it seems that case-based discussions serve as an effective instructional technique. This method fosters critical thinking and problem-solving abilities while facilitating collaboration by providing trainees with active involvement in real-life situations. Additionally, a flexible method that may be tailored according to the trainees’ needs.
Simulation training in healthcare is a valuable tool for enhancing professional proficiency and ensuring patient safety. This training method can be implemented through low and high-fidelity patient simulators, virtual reality, and standardized patients across diverse settings.14 Moreover, it facilitates the recognition and resolution of ethical concerns about multiple ethical principles, including autonomy, beneficence, justice, informed consent, nonmaleficence, fairness, truthfulness, advocacy, and dedication.15–20
In the study, two program directors with simulation fellowships were interviewed, and it was found that most training centers housed simulation facilities. However, these resources were often underutilized or only employed for role-playing exercises. Simulation is valuable for detecting ethical concerns about patient safety and fostering ethical knowledge transmission. Both technical and non-technical abilities are crucial for delivering competent care to patients. Incorporating ethical principles into simulation-based education is essential, and educators must utilize evidence-based approaches to improve trainees’ clinical decision-making21 while aligning with international standards.
While bedside education may serve as a highly validated teaching approach, particularly in daily clinical activities, it is unfortunate that some trainees were not encompassed within the medico-legal contexts. Their roles were limited to clerkship duties. As active team members, trainees should be incorporated into their patients’ ethical and legal considerations. This inclusion can be adapted according to their prior experiences and current level of training, ranging from observing trainers and senior trainees to seeking advice from ethical and legal experts within their training institutions.
Universally, experts suggested integrating essential bioethical and medical law principles in diverse methods and at various stages of medical education. This approach aims to produce graduates who adhere to legal and ethical guidelines, as emphasized by Stirrat, Johnston, Gillon, and Boyd22 and Von Fragstein et al.23 In relation to Muslim communities, the incorporation of Islamic moral and ethical principles into the medical curriculum has positively influenced student performance.24 This finding corroborates the perspectives of our study participants, who advocate for implementing a bioethical and legal module in SBEM, deeming it essential to meet the unique needs of our community.
Limitations
This study was conducted during the COVID-19 pandemic, and most emergency physicians were on the frontlines, preventing communications with a broader sample. There are other training programs in the Kingdom of Saudi Arabia where their program directors and trainees may have different perceptions and opinions.
Conclusion
The study indicated that the current educational initiatives in SBEM to cover the basic legal and bioethical subjects are suboptimal and far from the expectation of the two stakeholders. There are no clear learning objectives, combined practice, or even study guide to help the trainees develop safe approaches for the variable ethical and legal challenges they may face during their training.
It could be beneficial to have a comprehensive protocol that illustrates the essential required competencies, clear learning outcomes, a unique study guide as well as dedicated educators, to assist the trainees in understanding the principles and the guidelines of Islamic ethics and jurisprudence and provide them with a strong foundation for navigating ethical and legal dilemmas in the context of their practice. A well-designed module could help the trainees to identify and address potential issues from the Islamic perspective and ultimately promote the delivery of culturally sensitive and patient-centered care. Further studies to explore the practice in other training programs and additional steps to continue the needs assessment are recommended.
Funding
The study was self-funded, and the authors had no other sources of funding.
Disclosure
The authors have no conflicts of interest and were not involved in the SBEM curriculum development.
References
1. Balch CM, Oreskovich MR, Dyrbye LN, et al. Personal consequences of malpractice lawsuits on American surgeons. J Am Coll Surg. 2011;213(5):657–667. doi:10.1016/j.jamcollsurg.2011.08.005
2. Zajdel J, Zajdel R, Kuna P. Knowledge of medical law amongst doctors of internal diseases. Int J Occup Med Environ Health. 2013;26(2). doi:10.2478/s13382-013-0083-5
3. Todorovski N. Significance of medical law in medical school curriculum. Acta Med Median. 2018;57(3):60–65.
4. Chamsi-Pasha H, Albar MA. Islamic medical jurisprudence syllabus: a Review in Saudi Arabia. Med J Malaysia. 2017;72(5):279.
5. Ministry of Health, Kingdom of Saudi Arabia. Law of Practicing Healthcare Professions. Available from: https://www.moh.gov.sa/en/Ministry/Rules/Documents/Law-of-Practicing-Healthcare-Professions.pdf.
6. NHS Litigation Authority. NHS litigation authority annual report and accounts 2015/2016. Available from: https://www.gov.uk/government/publications/nhs-litigation-authority-annual-report-and-accounts-2015-to-2016Documents/NHS_Litigation_Authority_Annual_Report_and_Accounts_2015-2016.pdf.
7. Saudi Commission for Health Specialties. About Us. Available from: https://scfhs.org.sa/en/about-us.
8. Saudi Commission for Health Specialties. Training Programs. Available from: https://scfhs.org.sa/en/training?tid=29&dtid=43&page=2.
9. Frank JR The CanMEDS 2015 physician competency framework. The Royal College of Physicians and Surgeons of Canada; 2015. Available from: http://www.royalcollege.ca/rcsite/CanMEDS/CanMEDS-framework-e.
10. Saudi Commission for Health Specialties. Training and continuing professional development. Available from: https://scfhs.org.sa/en/training?tid=29&dtid=43&page=2.
11. Gupta S, Phatak A, Panchal D. Court room exposure to medical students: a practical approach to legal procedures in Indian scenario. J Forensic Leg Med. 2013;20(6):767–769. doi:10.1016/j.jflm.2013.05.004
12. Ivanović S, Stanojević Č, Jajić S, Vila A, Nikolić S. Medical law and ethics. Acta Med Median. 2013;52:3.
13. Campbell AT. Teaching law in medical schools: first, reflect. J Law Med Ethics. 2012;40(2):301–310. doi:10.1111/j.1748-720X.2012.00665.x
14. Göriş S, Bilgi N, Bayındır SK. Use of simulation in nursing education. Düzce Univ J Health Sci Inst. 2014;4:25–29.
15. Haddad A. What health science students learn from playing a standardized patient in a ethics course. Camb Q Healthc Ethics. 2010;19:481–487. doi:10.1017/S096318011000037X
16. Vanlaere L, Coucke T, Gastmans C. Experimental learning of empathy in a care-ethics lab. Nurs Ethics. 2010;17:325–336. doi:10.1177/0969733010361440
17. Hallenbeck VJ. Use of high-fidelity simulation for staff education/development. J Nurses Staff Dev. 2012;28:260–269. doi:10.1097/NND.0b013e31827259c7
18. Smith KV, Witt J, Klaassen J, Zimmerman C, Cheng A. High-Fidelity Simulation and legal/ethical concepts: a transformational learning experience. Nurs Ethics. 2012;19:390–398. doi:10.1177/0969733011423559
19. Vanlaere L, Timmermann M, Stevens M, Gastmans C. An explorative study of experiences of healthcare providers posing as simulated care receivers in a “care-ethical” lab. Nurs Ethics. 2012;19:68–79. doi:10.1177/0969733011412103
20. Smith KV, Klaassen J, Zimmerman C, Cheng A. Patient simulation learning experience to teach legal and ethical issues. J Prof Nurs. 2013;29:168–173. doi:10.1016/j.profnurs.2012.04.020
21. Pinar G, Peksoy S. Simulation-based learning in healthcare ethics education. Creat Educ. 2016;7:131–138. doi:10.4236/ce.2016.71013
22. Stirrat GM, Johnston C, Gillon R, Boyd K. Medical ethics and law for doctors of tomorrow: the 1998 consensus statement updated. J Med Ethics. 2010;36(1):55–60. doi:10.1136/jme.2009.034660
23. Von Fragstein M, Silverman J, Cushing A, et al. UK consensus statement on the content of communication curricula in undergraduate medical education. Med Educ. 2008;42(11):1100–1107. doi:10.1111/j.1365-2923.2008.03137.x
24. Jamilah J, Najib AA, Dzulkhairi M, Ariff H, Ismail NN. Integration of Islamic input in medical curriculum–Universiti Sains Islam Malaysia (USIM) experience. The Int Med J Malaysia. 2014;13(2):73–77.

